Avascular necrosis (AVN), also known as osteonecrosis, is a condition where bone tissue dies due to a lack of blood supply. Over time, this can cause the bone to collapse, leading to severe joint damage and arthritis. AVN most commonly affects the hip, but it can also occur in other joints like the knees and shoulders. With around 20,000 new cases diagnosed in the U.S. annually, this progressive condition is more likely to impact individuals between the ages of 30 and 65. Early detection and treatment are critical in preventing joint collapse and preserving mobility.
- What is Avascular Necrosis of the Hip?
- What are the Symptoms of Avascular Necosis?
- What Causes Avascular Necrosis?
- How is Avascular Necrosis Diagnosed?
- What are the stages of Avascular Necrosis of the Hip?
- When is Surgery needed for a Rotator Cuff Tear?
- What is the Prognosis for Avascular Neccrosis of the Hip?
Avascular necrosis of the hip causes significant hip and groin pain and can limit simple, everyday activities. It may occur following an injury but is often discovered in people with no prior history of injury to the hip.
What is Avascular Necrosis of the Hip
Osteonecrosis of the hip, also known as avascular necrosis (AVN), occurs when the blood supply to the femoral head—the ball of the ball-and-socket hip joint—is disrupted.
Without adequate blood flow, the bone tissue in the femoral head begins to die, causing the bone to weaken and eventually collapse.
As the condition progresses, the smooth cartilage covering the bone can also deteriorate, leading to severe arthritis.
Osteonecrosis is a progressive condition that typically affects individuals between the ages of 30 and 65, with men being more frequently diagnosed than women. In many cases, osteonecrosis can affect both hips.
Left untreated, this condition can severely limit mobility, causing intense pain and eventually requiring total hip replacement surgery. Early diagnosis is essential, as timely treatment can help slow the progression of the disease and prevent joint collapse.
What are the Symptoms of Avascular Necrosis of the Hip?
 Avascular necrosis (AVN) of the hip typically begins with mild or intermittent pain in the hip, groin, or buttock area.
Avascular necrosis (AVN) of the hip typically begins with mild or intermittent pain in the hip, groin, or buttock area.
In the early stages, this pain may only occur when putting weight on the affected joint, such as during walking or standing.
As the condition progresses, the pain becomes more persistent and may be felt even at rest or during the night.
Stiffness and a reduced range of motion in the hip joint develop over time, making it difficult to perform everyday activities like climbing stairs, bending, or getting out of a chair.
In advanced stages, the collapse of the femoral head can lead to more intense pain, significant limping, and difficulty bearing any weight on the affected leg.
Early symptoms can be subtle, which is why timely diagnosis and treatment are crucial to prevent further joint damage.
What Causes Avascular Necrosis of the Hip?
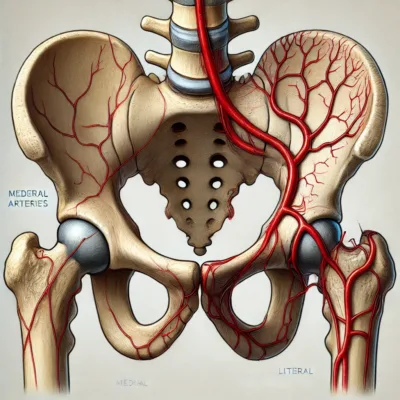 Avascular necrosis (AVN) of the hip occurs when the blood supply to the femoral head is disrupted, leading to the death of bone tissue. The causes of AVN can be divided into traumatic and atraumatic categories.
Avascular necrosis (AVN) of the hip occurs when the blood supply to the femoral head is disrupted, leading to the death of bone tissue. The causes of AVN can be divided into traumatic and atraumatic categories.
Traumatic causes typically involve injuries such as hip fractures or dislocations that damage the blood vessels supplying the femoral head. These injuries can severely reduce or block blood flow, causing bone cells to die and the bone to weaken. AVN may occur several years after a hip injury. It is commonly seen following a dislocation of the hip or a fracture involving the neck of the femur.
Atraumatic causes, on the other hand, are non-injury related and include underlying medical conditions or treatments. Long-term use of corticosteroids for conditions like asthma or lupus is one of the most common non-traumatic causes, although the exact reason these medications lead to AVN is unclear. Other medical conditions linked to AVN include sickle cell disease, lupus, diabetes, and cancer treatments like radiation therapy, which can impair blood flow to the bone.
Behavioral risk factors also play a significant role in the development of AVN. Excessive alcohol consumption is a leading behavioral cause, as it can lead to fatty deposits in the blood vessels, reducing circulation to the femoral head. Additionally, smoking constricts blood vessels, further limiting the blood supply to the bone. These lifestyle factors, combined with underlying health conditions, significantly increase the risk of AVN. Reducing alcohol intake, quitting smoking, and managing medical conditions are essential steps to lower the risk of developing AVN of the hip.
How is AVN of the Hip diagnosed?
 To diagnose AVN of the hip, doctors use physical exams and imaging tests.
To diagnose AVN of the hip, doctors use physical exams and imaging tests.
Exam
Your doctor will perform a physical exam, checking your range of motion and muscle strength. They’ll ask about your symptoms and perform tests to determine where the pain originates and how severe the pain is.
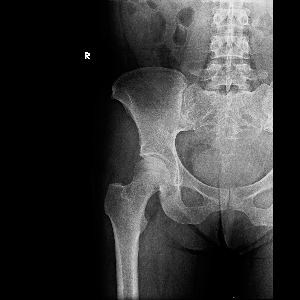
X-rays
Doctors often use X-rays to rule out other causes of hip or leg pain, such as a fracture or arthritis. Advanced AVN may be detected on X-rays, but early stages of AVN may not be detectable with X-rays.
MRI
An MRI is the most common test for diagnosing avascular necrosis. It provides detailed images of the bones in the hip and pelvis. Damaged areas of the bone can be identified and the size of the area affected can be measured.
What are the stages of AVN of the hip?
 Avascular necrosis (AVN) of the hip progresses through four stages, each representing the degree of bone damage and collapse. Staging helps doctors determine the severity of the condition and guides treatment decisions. The stages are assessed through clinical evaluation and imaging tests such as X-rays and MRIs.
Avascular necrosis (AVN) of the hip progresses through four stages, each representing the degree of bone damage and collapse. Staging helps doctors determine the severity of the condition and guides treatment decisions. The stages are assessed through clinical evaluation and imaging tests such as X-rays and MRIs.
Stage I: Pre-collapse (Early Stage)
- In the earliest stage, the bone appears normal on X-rays, but AVN has started to affect the femoral head. The patient may experience mild symptoms, such as intermittent pain, or no symptoms at all.
- Diagnosis: X-rays may appear normal, so an MRI is usually required to detect early changes in bone tissue. The MRI shows areas of bone with reduced blood supply before collapse begins.
- Treatment: Non-surgical treatments like core decompression, physical therapy, or medications may prevent progression.
Stage II: Early Bone Changes (Pre-collapse)
- At this stage, the bone starts to show small changes, such as increased density or sclerosis (hardening), but the femoral head has not yet collapsed. Pain becomes more noticeable, particularly during activity.
- Diagnosis: X-rays may now show subtle changes in the bone structure. MRI is still used for a clearer picture of how much bone is affected.
- Treatment: Core decompression and bone grafting can be considered to restore blood flow and prevent collapse.

Stage 3 AVN
Stage III: Collapse of the Femoral Head (Pre-arthritic)
- In Stage III, the femoral head starts to collapse, losing its rounded shape, and the overlying cartilage may begin to show signs of damage. Symptoms become more severe, including pain during both movement and rest, and there may be limited joint motion.
- Diagnosis: X-rays reveal the early signs of femoral head collapse, often showing a “crescent sign,” which indicates the formation of a fracture beneath the articular cartilage. An MRI further confirms the extent of collapse.
- Treatment: Surgical options, such as core decompression with or without stem cell therapy, or more invasive procedures like vascularized fibula grafts, may be required to preserve the hip joint.
Stage IV: Advanced Collapse and Osteoarthritis
- In this final stage, the femoral head has collapsed entirely, and the surrounding cartilage is severely damaged, leading to osteoarthritis. Patients experience chronic pain and significant loss of hip mobility.
- Diagnosis: X-rays clearly show the collapse of the femoral head and damage to the joint. MRI is used less frequently at this stage since X-rays provide sufficient information on the extent of the damage.
- Treatment: At this point, total hip replacement is often the only viable treatment to relieve pain and restore function.
How Staging is Performed
- Imaging Tests:
- X-rays are used to identify structural changes in the bone and detect collapse or arthritis.
- MRI is the most sensitive imaging technique for early detection, as it shows bone changes before they appear on X-rays.
- In some cases, CT scans or bone scans are used to gather additional information.
Proper staging of AVN helps in selecting the appropriate treatment plan to prevent joint collapse and alleviate pain, with early intervention providing the best chance for joint preservation.
What Treatments are available for Avascular Necrosis?
The treatment options for avascular necrosis (AVN) of the hip depend on the stage of the disease, the amount of bone damage, and the patient’s overall health. The primary goal of treatment is to improve blood flow to the affected bone, reduce pain, and prevent further joint collapse. Early diagnosis provides more opportunities to preserve the natural hip joint, while advanced cases may require surgical interventions like hip replacement. Here’s a detailed look at the treatment options available:
1. Non-Surgical Treatments for Early-Stage AVN
Non-surgical treatments are most effective when AVN is diagnosed in the early stages before the femoral head has collapsed. These treatments focus on pain relief and slowing the progression of the disease but are unlikely to reverse bone damage.
- Rest and Activity Modification: The use of crutches or canes can help minimize stress on the hip, and may provide temporary relief of pain. Avoiding high impact activities like running or jumping also reduces the stress on the weakened hip joint. While this may provide short-term relief of pain, it is not a great long-term solution.
- Medications:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs like ibuprofen or naproxen are often prescribed to manage pain and inflammation in the affected hip joint.
- Bisphosphonates: These medications are sometimes used to slow bone damage, but their effectiveness in AVN treatment is still under investigation.
- Blood Thinners: In some cases, anticoagulants may be prescribed if the AVN is related to blood clotting disorders, as these can improve blood flow to the hip.
- Physical Therapy: Targeted exercises can improve the range of motion, strengthen the surrounding muscles, and enhance joint stability. However, weight-bearing exercises are typically avoided to reduce stress on the hip.
- Hyperbaric Oxygen Therapy (HBO): HBO involves breathing pure oxygen in a pressurized chamber, which increases oxygen levels in the blood. This therapy has been used to stimulate bone healing by promoting blood flow to the femoral head. While promising, it is not a widely established treatment for AVN and is typically used in conjunction with other therapies.
2. Surgical Treatments for Advanced AVN
As AVN progresses and bone damage worsens, surgical interventions become necessary to preserve or restore hip function. The choice of surgery depends on the stage of AVN, the extent of the bone collapse, and the patient’s overall health.
- Core Decompression: This minimally invasive surgery is often used in early-stage AVN to relieve pressure within the femoral head and promote blood flow. The surgeon drills small holes into the bone to decrease pressure and create channels for new blood vessels to form, allowing the bone to heal. Core decompression is sometimes combined with stem cell therapy or bone grafting to encourage new bone growth. This procedure is most successful before the femoral head has collapsed, and patients typically experience pain relief and improved hip function.
- Bone Grafting:
- Non-vascularized Bone Grafting: This procedure involves transplanting healthy bone from another part of the body or using synthetic bone material to replace damaged bone in the femoral head.
- Vascularized Fibula Grafting: In this more advanced technique, a section of the fibula (a bone in the lower leg) along with its blood supply is transplanted into the femoral head. The attached blood vessels are reconnected to improve blood flow to the area. This procedure is more invasive and requires a longer recovery period, but it can be highly effective in preventing further bone collapse when done early.
- Osteotomy: In an osteotomy, the surgeon cuts and reshapes the femur to shift the weight-bearing load away from the damaged part of the femoral head onto healthier bone. This procedure is less common and usually reserved for younger patients with early-stage AVN. Osteotomy can delay the need for hip replacement, but it is not always effective in preventing further progression of the disease.
- Total Hip Replacement (Arthroplasty): When AVN has advanced to the point where the
 femoral head has collapsed or severe arthritis has developed, total hip replacement becomes the most effective treatment option. In this procedure, the damaged femoral head and acetabulum (hip socket) are removed and replaced with artificial components made of metal, ceramic, or plastic. Total hip replacement surgery is highly successful in relieving pain and restoring mobility. However, patients are often advised to avoid high-impact activities to preserve the lifespan of the artificial joint, which typically lasts 15 to 20 years before needing revision surgery.
femoral head has collapsed or severe arthritis has developed, total hip replacement becomes the most effective treatment option. In this procedure, the damaged femoral head and acetabulum (hip socket) are removed and replaced with artificial components made of metal, ceramic, or plastic. Total hip replacement surgery is highly successful in relieving pain and restoring mobility. However, patients are often advised to avoid high-impact activities to preserve the lifespan of the artificial joint, which typically lasts 15 to 20 years before needing revision surgery.
3. Experimental and Emerging Treatments
As research into AVN continues, newer treatments are being explored to improve outcomes and prevent joint collapse.
- Stem Cell Therapy: In combination with core decompression, stem cell therapy involves harvesting stem cells from the patient’s bone marrow and injecting them into the femoral head to encourage new bone growth. This approach has shown promising results in improving hip function and reducing the progression of AVN.
- Growth Factors: Experimental treatments using growth factors to stimulate blood vessel formation and bone regeneration are under investigation. These biologic therapies aim to enhance the body’s natural healing process and improve blood flow to the affected bone.
4. Post-Surgical Rehabilitation and Recovery
Regardless of the type of surgery, post-surgical rehabilitation is crucial for successful recovery. Patients typically use crutches or walkers for several weeks after surgery to reduce weight-bearing on the operated hip. A personalized physical therapy program helps restore strength, flexibility, and range of motion. Full recovery can take several months, but most patients experience significant pain relief and improved mobility.
5. Long-Term Management and Follow-Up
Patients with AVN, particularly those who undergo hip-preserving surgeries, require regular follow-up visits to monitor the condition and ensure the treatment’s success. Preventive measures, such as avoiding high-impact activities and maintaining a healthy lifestyle, are essential to prolong joint health and minimize the risk of further complications.
What is the prognosis for AVN of the hip?
The prognosis for avascular necrosis (AVN) of the hip largely depends on the stage at which the condition is diagnosed and the effectiveness of treatment.
Early diagnosis offers the best chance for positive outcomes, as interventions such as core decompression and other hip-preserving procedures can prevent or slow the progression of the disease. In these cases, patients may experience significant pain relief and maintain hip function, avoiding joint collapse.
However, if AVN is diagnosed after the femoral head has begun to collapse (Stage III or IV), the prognosis worsens. Advanced stages typically lead to severe arthritis and joint destruction, requiring a total hip replacement. Fortunately, hip replacement surgery has a high success rate, with most patients experiencing significant pain relief and restored mobility. Prosthetic hips generally last 15 to 20 years, though further surgeries may be needed as the artificial joint wears down over time.
Factors that can negatively impact the prognosis include larger areas of bone damage, delayed diagnosis, and underlying health conditions like diabetes or lupus. Additionally, lifestyle factors such as smoking and excessive alcohol use can worsen the condition and slow recovery.
Ultimately, early intervention and appropriate treatment are key to improving long-term outcomes for patients with AVN of the hip.
Definitely the best decision I’ve ever made was seeking the expert services of Dr. Davis. It’s been years since I’ve been able to move my arm/shoulder in certain directions. I’m still in the mist of my healing, but hands down the best service!
Very knowledgeable and supportive staff. Dr. Davis spends time to understand and explain, my experience through surgery and recovery of torn rotator cuff, labrum, and bicep was outstanding.
Excellent surgeon. My husband needed shoulder repair and Dr. Davis did a great reconstruction surgery. Very good at explaining the details of what needed to be done and how he did it post surgery. He gave realistic expectations and paid close attention to the progress for the PT.
